The landscape of personal health management is undergoing a profound transformation, driven by the rapid evolution of wearable health monitors. These sophisticated devices have advanced far beyond simple step-counting, moving into the realm of clinical-grade health metrics. From high-tech smartwatches and discreet rings to specialized biosensors and intelligent patches, these new-generation wearables are enabling continuous, real-time, and personalized health tracking. This shift empowers individuals to take unprecedented control over their well-being and is fundamentally reshaping the future of preventive and chronic healthcare.
The market for these devices is experiencing explosive growth, fueled by rising global awareness of lifestyle diseases, the demand for remote patient monitoring (RPM), and the seamless integration of Artificial Intelligence (AI) into data analysis. The goal is no longer just fitness—it is the integration of everyday health data into a cohesive, actionable, and potentially life-saving healthcare ecosystem. This detailed exploration delves into the cutting-edge technologies, advanced monitoring capabilities, key applications, and the ethical considerations defining the next chapter of digital health.
Advanced Biosensing and Monitoring Capabilities

The core of the wearable health revolution lies in the sophistication of its biosensors and the range of physiological data they can capture. Modern devices integrate an array of high-accuracy sensors that provide continuous, long-term data far superior to the “snapshot” readings traditionally taken during a doctor’s visit.
A. Cardiovascular Monitoring Innovations
Monitoring heart health remains a critical application for wearable technology, with capabilities now mirroring those of clinical devices.
- Electrocardiogram (ECG) Functionality: While earlier models focused on basic heart rate (HR), modern smartwatches and rings offer on-demand ECG readings. This allows users to check for signs of Atrial Fibrillation (AFib) and other irregular heart rhythms. Advanced algorithms, sometimes even with regulatory approval, are being developed to detect complex conditions like Left Ventricular Systolic Dysfunction (LVSD).
- Heart Rate Variability (HRV) Analysis: HRV, the subtle fluctuation in the time interval between consecutive heartbeats, is a crucial indicator of the body’s autonomic nervous system balance, stress levels, and recovery status. Wearables provide continuous HRV data, enabling personalized recovery and training recommendations.
- Continuous Blood Pressure Monitoring: This has long been a challenge for wrist-worn devices. However, new non-invasive technologies, including tiny ultrasound sensors and advanced photoplethysmography (PPG) combined with AI, are pushing closer to cuff-level accuracy for real-time, convenient blood pressure tracking.
B. Respiratory and Oxygen Metrics
The pandemic accelerated the adoption and refinement of sensors tracking respiratory health.
- Blood Oxygen Saturation (): Pulse oximetry, which measures the percentage of oxygen-carrying hemoglobin in the blood, is now a standard feature. Continuous monitoring is vital for conditions like Sleep Apnea and monitoring overall respiratory function.
- Respiratory Rate (RR): Tracking breaths per minute, especially during sleep, provides important context for overall health and can serve as an early warning sign for infections or other systemic changes.
C. Metabolic and Chemical Analysis
Breaking the barrier of traditional lab tests, next-generation wearables are starting to analyze biochemical markers.
- Continuous Glucose Monitors (CGMs): Initially patches worn on the skin, CGMs for managing diabetes offer real-time glucose readings without the need for finger pricks. Integration with smartwatches and insulin pumps makes diabetes management more seamless and proactive.
- Non-Invasive Glucose Sensing: The ultimate goal—a completely non-invasive, wrist-based glucose monitor—is on the horizon. Companies are investing heavily in technologies like Raman spectroscopy and advanced optical sensors to achieve this landmark feature.
- Stress and Hydration Monitoring: Devices are incorporating sensors to analyze cortisol levels in sweat (a stress hormone), as well as electrolyte composition to provide real-time hydration alerts and stress management guidance.
The Power of Artificial Intelligence and Data Analytics

The true leap in wearable technology isn’t just in the data collection, but in the intelligence used to interpret that data. The integration of AI and Machine Learning (ML) is transforming raw sensor readings into actionable, personalized health insights.
A. Predictive Health and Early Detection
AI algorithms constantly analyze the vast datasets collected by the wearable (heart rate, sleep stages, temperature trends, activity patterns) to identify subtle deviations from a user’s personal baseline.
- Forecasting Illness: A persistent change in resting heart rate or a slight elevation in skin temperature, undetectable by the user, can be flagged by AI as a potential early indicator of an impending cold, flu, or other infection, allowing for proactive rest and intervention.
- Predictive Alerts: For patients with chronic conditions, AI can predict the likelihood of an asthma attack, a hypertension crisis, or a blood sugar spike, allowing the user or caregiver to intervene before an emergency occurs.
B. Personalized Coaching and Lifestyle Optimization
AI goes beyond simply alerting users to problems; it actively assists in improving daily habits and overall healthspan.
- Sleep and Recovery Guidance: Advanced sleep trackers use AI to analyze time spent in various sleep stages (REM, deep, light) and cross-reference it with daytime strain and HRV data. The device then offers personalized recommendations for optimal bedtime, recovery activities, and sleep environment adjustments.
- Exercise Optimization: AI coaches can generate tailored workout plans, adjust intensity based on the user’s current recovery status, and even offer real-time feedback on form or heart rate zones, maximizing the effectiveness of every session.
C. Enhanced Data Security and On-Device Processing
With more sensitive data being collected, security is paramount. The trend is toward on-device intelligence, where complex analysis is performed locally on the wearable’s microprocessors. This minimizes the need to send massive amounts of raw, highly personal data to the cloud, enhancing privacy and increasing the speed of real-time alerts.
Transforming Healthcare Delivery
The new generation of wearable health monitors is no longer just a consumer novelty; it is an indispensable component of the modern healthcare system, particularly in the fields of Remote Patient Monitoring (RPM) and chronic disease management.
A. Remote Patient Monitoring (RPM)
RPM leverages wearables to continuously track patients outside of traditional clinical settings, dramatically improving care for those with chronic diseases like hypertension, diabetes, and heart failure.
- Reduced Hospitalizations: Continuous data allows doctors to spot deteriorating conditions early and adjust medication or treatment plans remotely, preventing costly emergency room visits and readmissions.
- Comprehensive Data for Clinicians: Physicians gain a far richer, more longitudinal view of a patient’s health than is possible from brief in-office checkups. This data leads to more informed diagnoses and highly personalized treatment.
- Increased Patient Engagement: By actively tracking their own data and seeing the direct impact of lifestyle changes, patients become more engaged and compliant with their treatment protocols.
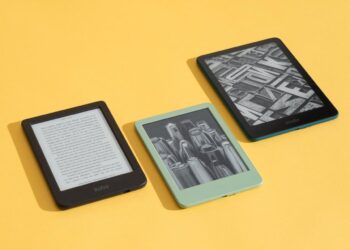
B. Specialization Beyond the Wrist
While smartwatches dominate the market, specialized, discreet devices are addressing specific health needs with greater accuracy and wearability.
- Smart Rings: These non-obtrusive devices, worn on a finger, often provide superior accuracy for sleep and heart rate tracking due to their placement against a major artery. Their smaller size and longer battery life make 24/7 wear more appealing to many users.
- Smart Patches and Electronic Tattoos: These are ultra-thin, adhesive sensors worn directly on the skin for days or weeks. They are typically used for specific, temporary clinical monitoring, such as extended ECG recording or constant hydration tracking in professional athletes.
- Smart Clothing (Textiles): Garments embedded with minute sensors offer comfortable, large-area data collection, monitoring everything from posture and muscle activity to core body temperature during intense activity.
Challenges and Future Directions
The immense potential of advanced health wearables comes with a set of critical hurdles that must be overcome for widespread, equitable adoption.
A. Accuracy and Regulatory Scrutiny
- Clinical Validation: While consumer devices are increasingly capable, their accuracy still needs to be validated against medical-grade standards, especially for diagnostics. Regulatory bodies like the FDA are creating new clearance pathways specifically for these devices, necessitating rigorous testing and clinical trials.
- Inclusivity and Bias: Sensor accuracy can be affected by factors such as skin tone, sweat, movement, and tattoos. Manufacturers must work to ensure their technology is equally accurate and reliable for all users, preventing algorithmic bias in health recommendations.
B. Data Privacy and Ownership
- Sensitive Health Data: Wearables collect some of the most sensitive personal data possible. Users must have transparent control over how their data is stored, analyzed, and shared with third parties, including researchers, insurers, and employers.
- HIPAA and GDPR Compliance: As wearable data integrates into the formal healthcare system (Electronic Health Records), strict adherence to international health data privacy regulations is non-negotiable.
C. Interoperability and Ecosystem Integration
- Seamless Data Flow: The vast amounts of data collected are only useful if they can be easily and securely integrated with existing hospital and physician Electronic Medical Record (EMR) systems. Lack of uniform standards for data sharing remains a major barrier.
Conclusion
The new wearable health monitors represent a paradigm shift from reactive medicine to proactive wellness. They are empowering billions to become the primary stakeholders in their own health, providing continuous, granular insight into the complex workings of the human body. The current generation of devices, powered by high-accuracy biosensors and sophisticated AI, is moving beyond fitness tracking to deliver genuine, clinically significant health metrics like ECG, , and soon, non-invasive glucose monitoring.
The impact of this technology is multifaceted: it is a democratization of health data, placing powerful diagnostic tools directly into the hands of consumers; it is the backbone of Remote Patient Monitoring, offering physicians the longitudinal data needed to manage chronic diseases more effectively and reduce the strain on hospital systems; and it is a key component in the push for longevity and personalized healthspan optimization.
However, the future success of this technology hinges on overcoming critical challenges, most notably ensuring clinical-grade accuracy for all users, guaranteeing robust data privacy, and establishing seamless interoperability with the existing healthcare infrastructure. As manufacturers, regulators, and healthcare providers collaborate, the evolution of wearable technology promises a future where health monitoring is constant, preventative, and deeply integrated into the fabric of everyday life, truly allowing us to monitor, understand, and ultimately optimize our own biology. This revolution is not just about a new gadget; it is about building a smarter, healthier, and more engaged global community. The promise is clear: to detect the whisper of illness before it becomes a shout, transforming the way we live and care for ourselves, one heartbeat and one step at a time.